Book Appointment Now
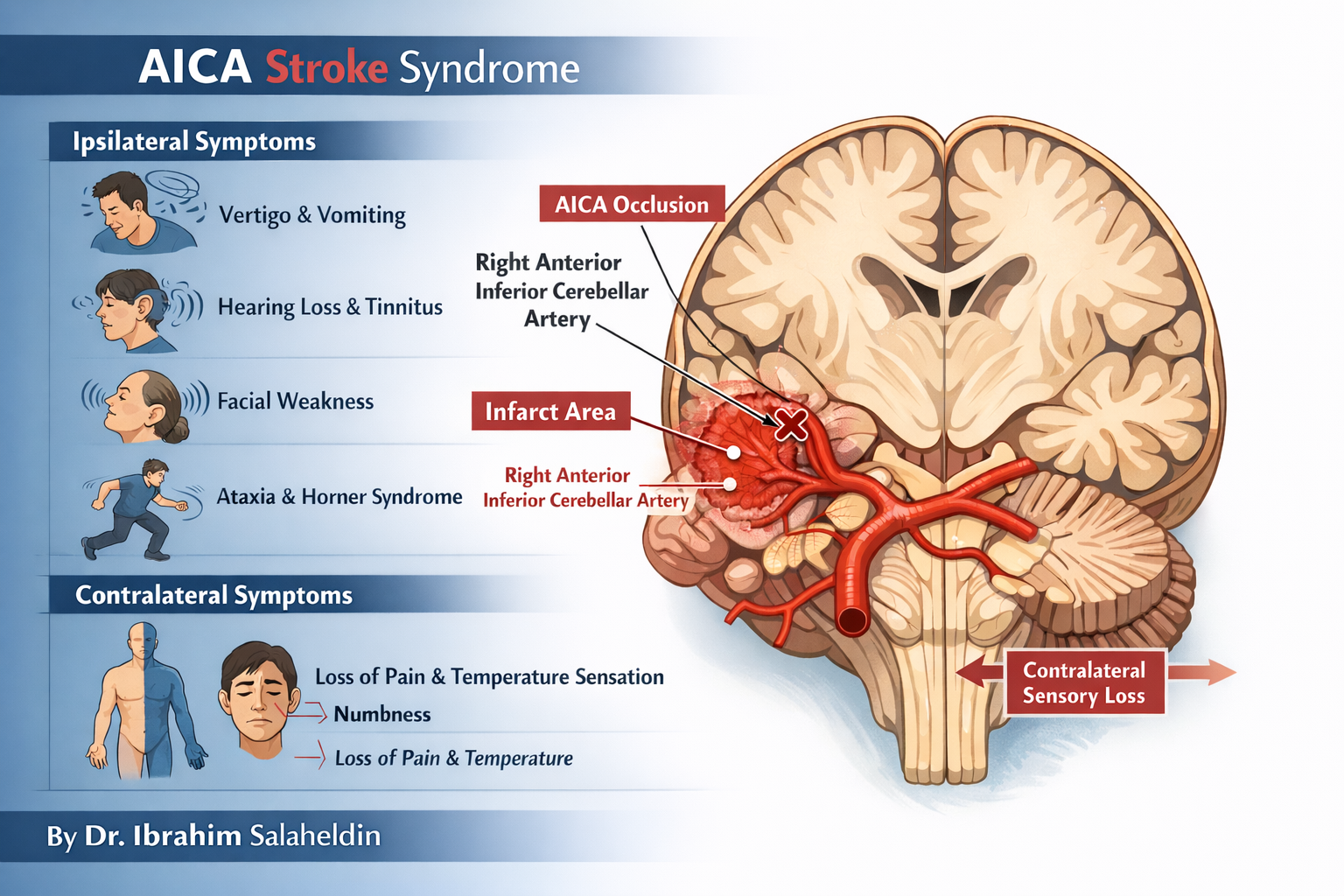
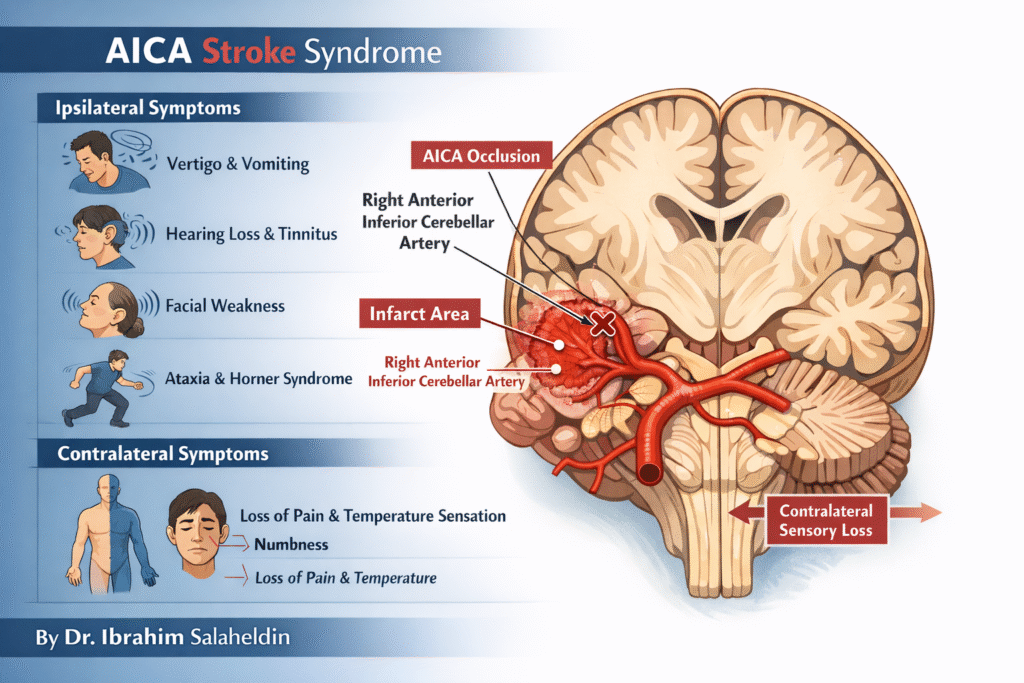
AICA Stroke Syndrome (Lateral Inferior Pontine Syndrome)
Author: Dr Ibrahim Elpum
Introduction
AICA stroke is a classic brainstem syndrome frequently tested in MRCP, USMLE, and medical school exams. When you understand the underlying neuroanatomy, the clinical features stop being confusing and start making perfect sense. This article breaks the topic down in a clear, exam-focused way.
Vascular Anatomy (Concept First)
The AICA is a branch of the basilar artery supplying:
- Lateral inferior pons
- Middle cerebellar peduncle
- Cerebellar hemisphere (anterior–inferior part)
- Facial nucleus (CN VII)
- Vestibulocochlear nucleus (CN VIII)
- Spinal trigeminal nucleus
- Spinothalamic tract
- Sympathetic fibres
When AICA is occluded → all structures in this territory malfunction → clinical pattern emerges.
Core Clinical Pattern
AICA stroke produces:
Ipsilateral cranial nerve signs + ipsilateral cerebellar signs + contralateral body sensory loss
This happens because:
- Cranial nerve nuclei are affected before decussation → ipsilateral signs
- Long tracts (e.g. spinothalamic) are affected after crossing → contralateral body signs
Ipsilateral Features (Same side as lesion)
These are the clues that localise the lesion to the pons and AICA territory:
1. Vertigo, vomiting, nystagmus
→ Involvement of vestibular nuclei (CN VIII)
2. Hearing loss and tinnitus
→ Involvement of cochlear nucleus (CN VIII)
This is a key feature that helps distinguish AICA from PICA
3. Lower motor neurone facial weakness
→ Involvement of facial nucleus (CN VII)
→ Facial droop, loss of nasolabial fold, inability to close eye
4. Loss of corneal reflex (afferent limb intact, efferent affected)
→ CN V sensory preserved, but CN VII motor impaired
5. Cerebellar ataxia
→ Involvement of middle cerebellar peduncle
→ Ipsilateral limb incoordination, gait instability
6. Ipsilateral Horner syndrome
→ Involvement of sympathetic fibres
→ Ptosis, miosis, anhidrosis
Contralateral Features (Opposite side of body)
Loss of pain and temperature over body
→ Involvement of spinothalamic tract
→ Contralateral loss of pain and temperature from trunk and limbs
The High-Yield Comparison: AICA vs PICA
| Feature | AICA | PICA |
|---|---|---|
| Facial weakness (LMN) | Yes | No |
| Hearing loss / tinnitus | Yes | No |
| Nucleus ambiguus (dysphagia, hoarseness) | No | Yes |
| Vertigo, nystagmus | Yes | Yes |
| Ataxia | Yes | Yes |
| Horner syndrome | Yes | Yes |
One-line exam pearl:
If there is facial paralysis + hearing loss, think AICA, not PICA.
How to Visualise It Clinically
Imagine the lesion sitting in the right lateral pons:
- Right face droops (CN VII)
- Right ear loses hearing (CN VIII)
- Right limb is ataxic (cerebellum)
- Right pupil is small (Horner)
- Left side of body loses pain and temperature (spinothalamic)
Suddenly the pattern becomes logical rather than memorised.
Why This Matters Clinically
Recognising posterior circulation strokes like AICA is critical because:
- They are often misdiagnosed as vertigo
- They can deteriorate rapidly
- Early stroke recognition improves outcomes
Any patient with:
Vertigo + facial weakness + hearing symptoms = brainstem stroke until proven otherwise
Final Take-Home Message
AICA stroke is a beautiful example of applied neuroanatomy:
- Ipsilateral facial weakness
- Ipsilateral hearing loss
- Ipsilateral ataxia
- Ipsilateral Horner syndrome
- Contralateral pain/temperature loss from body
If you understand the anatomy, the syndrome explains itself.
Written by Dr Ibrahim Elpum